Sexual Health Topics
- All Main Topics
- Men’s Sexual Health
- Women’s Sexual Health
- Cancer & Sexual Health (Oncosexology)
- Medications & Sexual Health
- Mental Health & Psychology
- Sexual Health Management & Treatments
- Sexual Orientation & LGBTQIA+ Health
- Sexually Transmitted Infections/Diseases (STIs/STDs)
Men’s Sexual Health
Many factors play a role in a man's sexual health. Here you can read articles on subjects like erectile dysfunction, Peyronie's disease, low testosterone, prostate-related sexual health issues, ejaculatory and orgasmic disorders, sexual pain, and other men's sexual health topics.
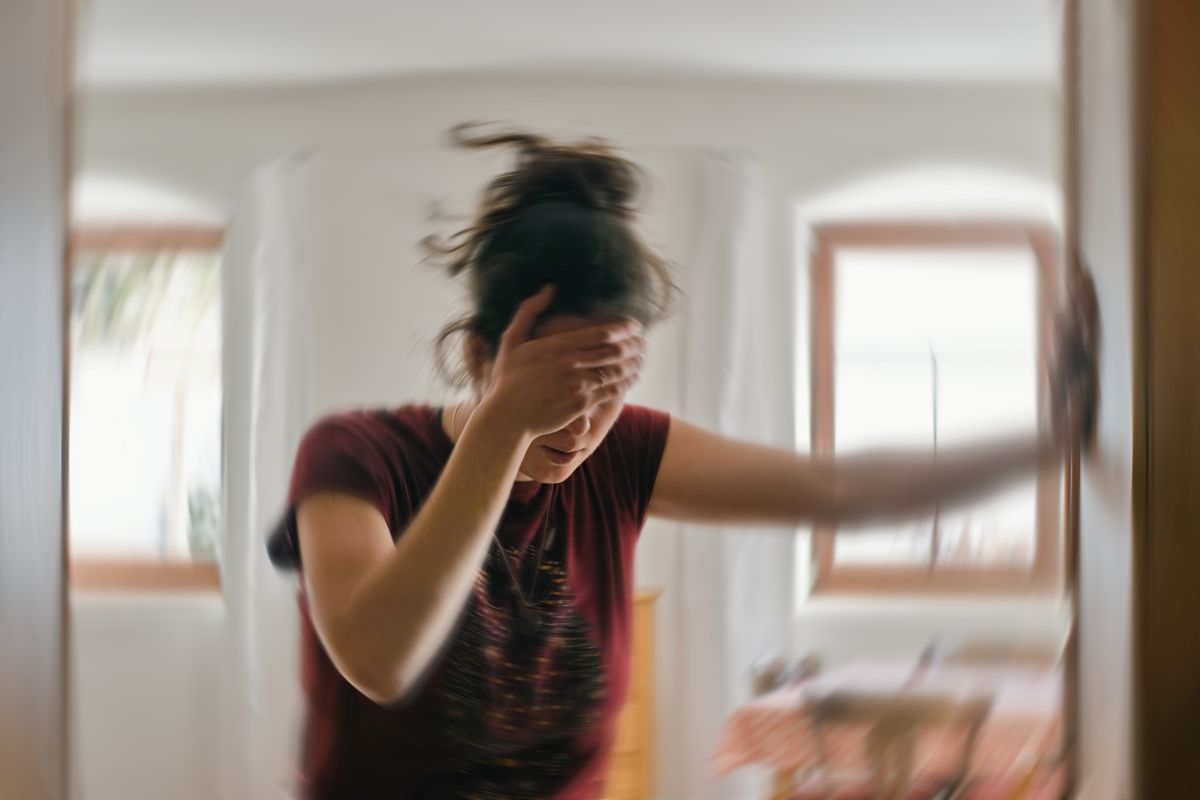
Women’s Sexual Health
A woman's sexual health can be affected by various conditions and circumstances. Find articles on sexual pain in women, menopause-related sexual health issues, arousal disorders, desire disorders, hormone therapy, orgasmic disorders, and other women's sexual health topics here.
Latest Articles
Cancer & Sexual Health (Oncosexology)
There are several different types of cancer, including those that can affect a person's genitals, breasts, or reproductive organs. Cancer of any kind and cancer treatments can have an impact on one's sexual health. Learn more about cancer and sexual health by clicking here.
Medications & Sexual Health
Did you know that medications like antidepressants, high blood pressure medications, birth control pills, and others can affect a person's sexual health? Find more information on the connection between medications and sexual health by clicking here.
Latest Articles
Mental Health & Psychology
Mental health can play a large role in one's sexual health. Explore topics such as desire discrepancy, sexual trauma, sexual abuse, fantasies, paraphilias, and paraphilic disorders here.
Latest Articles
Sexual Health Management & Treatments
Treatments for sexual health conditions vary as widely as the conditions themselves. Here you can discover more information on pharmaceuticals, hormone therapy, physical therapy, psychotherapy, aiding devices, lifestyle changes, surgical management, and other treatment options.
Latest Articles
Sexual Orientation & LGBTQIA+ Health
Gender identity and sexual orientation are important aspects of one's sexual health. Find information on sexual orientation, gender-affirming hormone therapy, gender-affirming surgery, and transition-related psychological care in these articles.
Latest Articles
Sexually Transmitted Infections/Diseases (STIs/STDs)
Sexually transmitted infections (STIs) are spread from one person to another during vaginal, anal, and oral sex. Learn more about STIs and STI prevention measures here.